Effects Of Diabetes On The Retina
Diabetes damages small blood vessels in the retina. Patients with diabetes may have:
-
A normal, healthy retina
-
Microscopic abnormalities that are visible on examination and signs of early disease, but which do not do not require treatment
-
Abnormalities in the retina that may or may not impact vision currently but require treatment in the office to prevent risk of severe vision loss
-
Abnormalities in the retina with vision decrease or loss that require surgery
The only way to distinguish between the above entities is to undergo a careful, dilated retinal examination by an experienced eye doctor. Timely, effective diagnosis and treatment of diabetic retinopathy is highly effective at maintaining vision and preventing vision loss.

Different Types Of Diabetic Retinal Disease (Diabetic Retinopathy)
The 2 main categories of diabetic retinopathy are non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
-
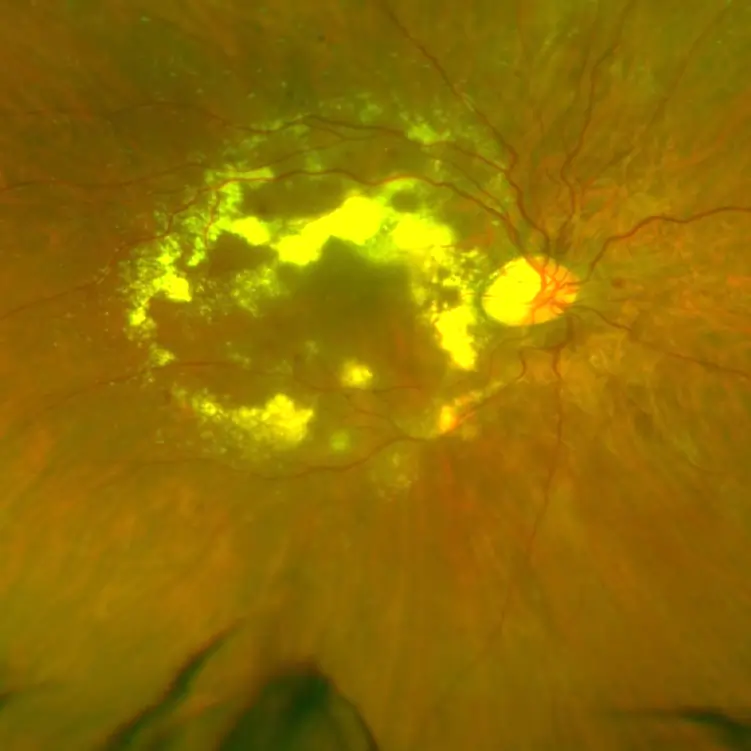
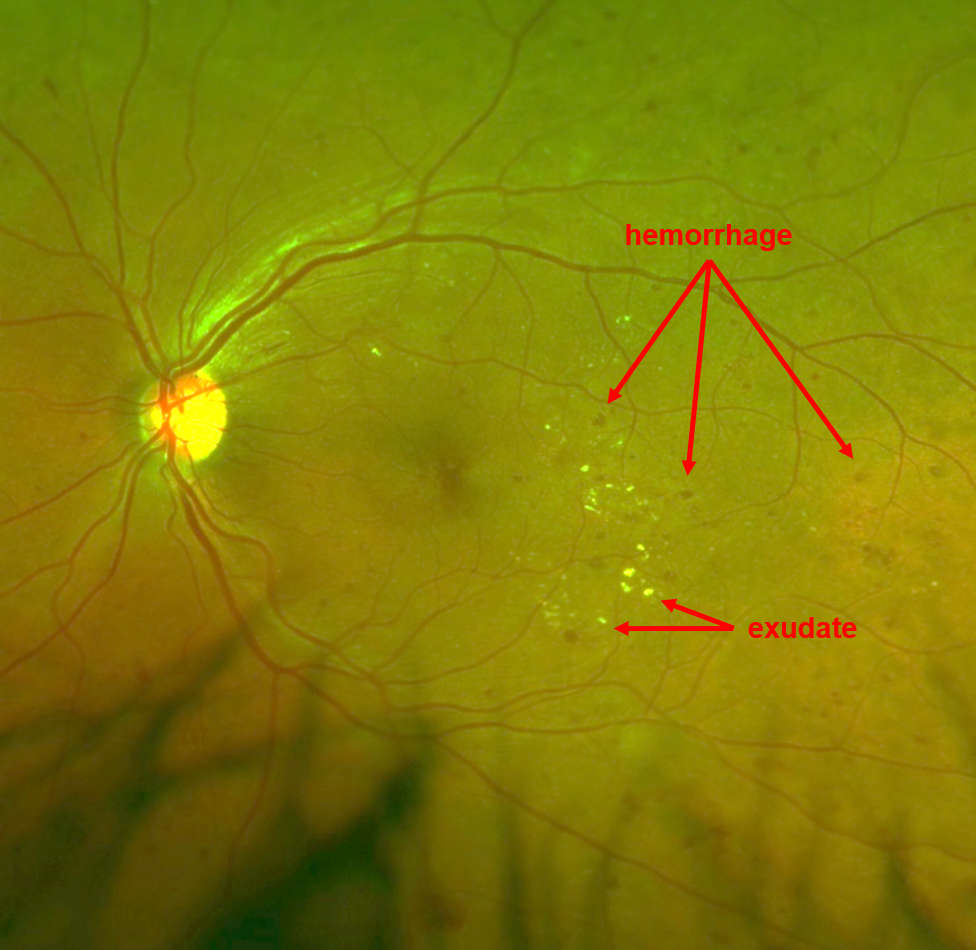
Non-Proliferative Diabetic Retinopathy (NPDR)
Among the first signs of diabetic retinopathy are microaneurysms, which are small red “blood dots” or hemorrhages that indicate pouches in the retinal capillaries and arteries (small blood vessels). These pouches leak serum or fluid from the bloodstream into the retina called exudates, which may cause it to swell. This swelling of the retina is known as macular edema. As retinopathy progresses, white spots in the retina, known as cotton-wool spots, may also develop which suggests lack of oxygen or blood flow. The swelling of the macula (diabetic macular edema) is the most common reason a patient with Diabetes will notice blurred central vision. Vision loss can range from mild to severe because of diabetic macular edema (DME).
-
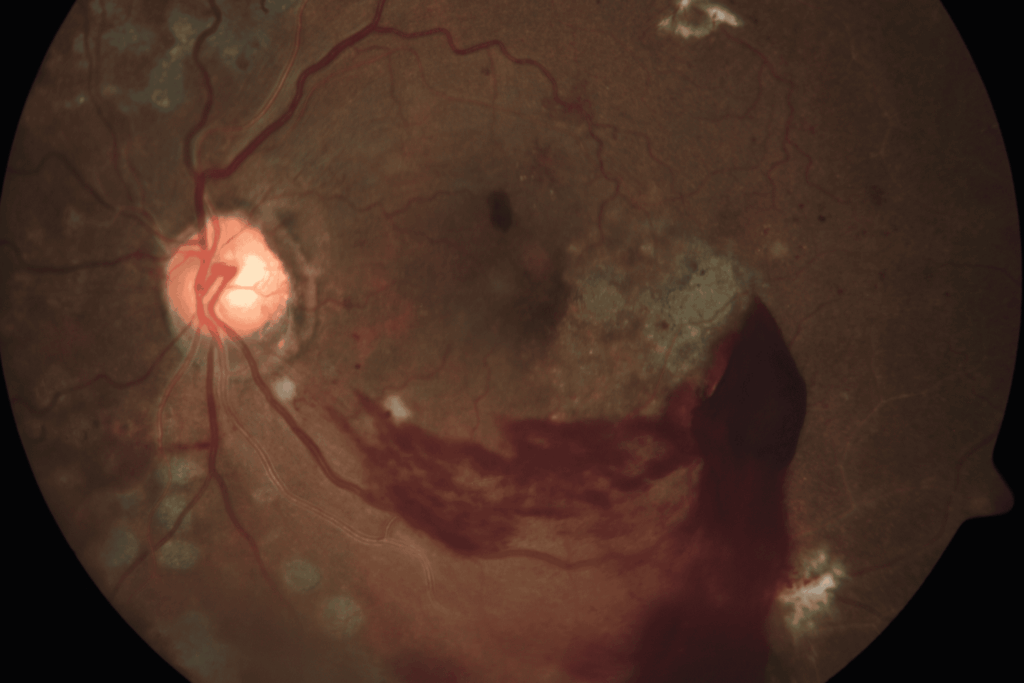
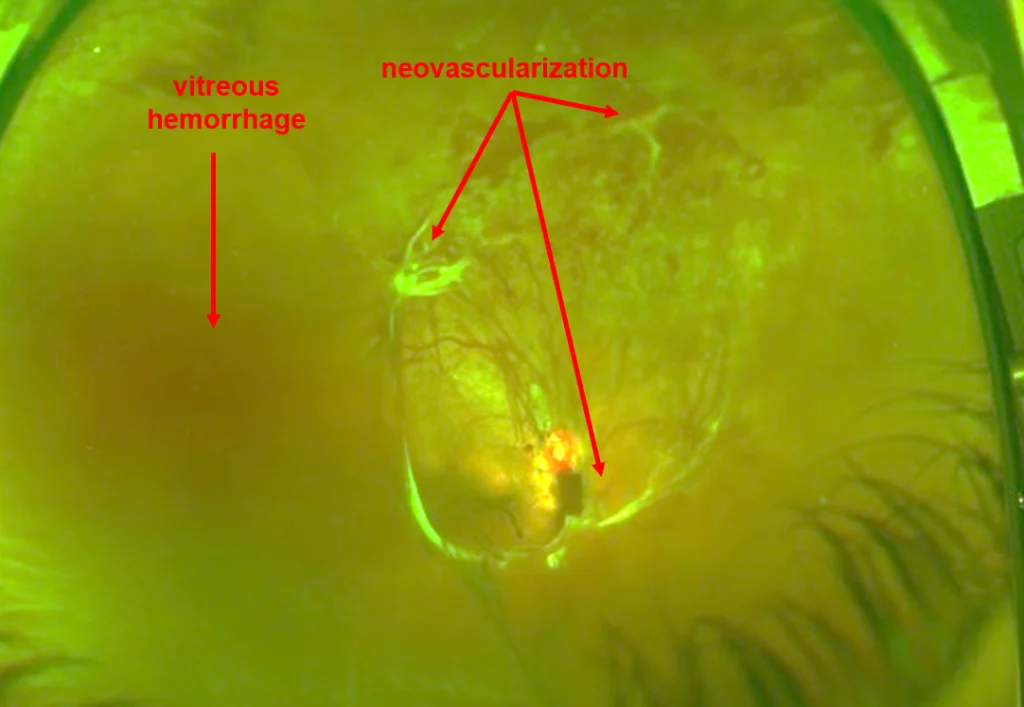
Proliferative Diabetic Retinopathy (PDR)
In some patients, diabetic retinopathy may progress from non-proliferative to proliferative. Proliferative diabetic retinopathy is characterized by neovascularization (neo = “new” and vascularization = “blood vessels”). That is, the appearance of new, fragile blood vessels on the optic nerve or retina’s surface. These new blood vessels frequently bleed into the vitreous cavity, causing hemorrhage. Furthermore, they may cause scarring on the retina, which can pull the retina, causing tractional retinal detachment. These new blood vessels are like “weeds in the garden” and may even grow in the front of the eye on the iris, causing a severe type of glaucoma to develop.
Unfortunately, the new blood vessels do not replace lost blood flow. Rather, they grow on the surface of the retina and cause vision loss in one of two ways:
Vitreous hemorrhage: A vitreous hemorrhage is bleeding into the eye. Instead of being filled with clear fluid through which one can see, the back of the eye is filled with blood, causing vision loss.
Tractional retinal detachment: The new blood vessels pull on the retina (create “traction”) and pull the retina off the eye wall (“retinal detachment”). The photoreceptors in detached retina cannot see and undergo damage, resulting in severe vision loss, sometimes irreversible vision loss
-
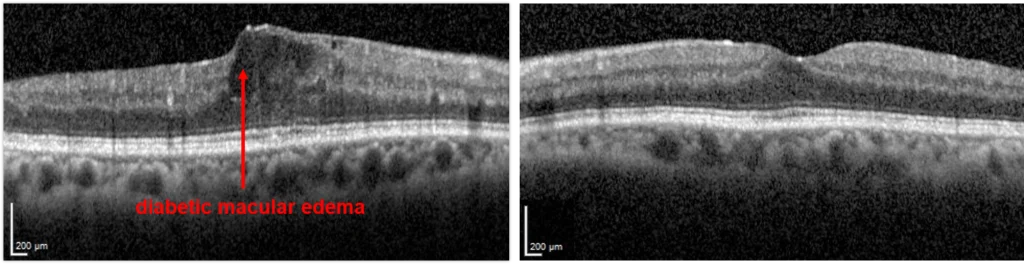
Diabetic Macular Edema (DME)
Patients with either NPDR or PDR may develop diabetic macular edema, otherwise known as swelling. Blood vessels damaged by diabetes are leaky, and the fluid that leaks from these vessels accumulate in the retina.
The macula is the centermost part of the retina, which is responsible for much of high quality vision. When diabetes causes swelling in the macula, one has “diabetic macular edema.”
The Warning Symptoms Of Diabetic Retinopathy
Often those diagnosed with diabetic retinopathy have normal vision, particularly when there is no diabetic macular edema, vitreous hemorrhage or tractional retinal detachment. This is precisely why regular eye examinations are important and can yield the most effective treatment because early detection is extremely vital.
When patients do exhibit symptoms, they often begin with blurred vision. Patients may also begin to see floaters, which may be signs of a vitreous hemorrhage.
The Causes Of Diabetic Retinopathy
Generally, diabetic retinopathy is caused by damage to the retinal blood vessels as a result of elevated sugar (glucose) levels in the bloodstream. Chronic elevated glucose levels may damage normal retinal blood vessels, causing them to leak fluid or create small hemorrhages in the retina. In more advanced stages, the retinal blood vessels can become blocked, restricting the retina’s oxygen levels. As a reaction to this, the retina grows new blood vessels or neovascularization.
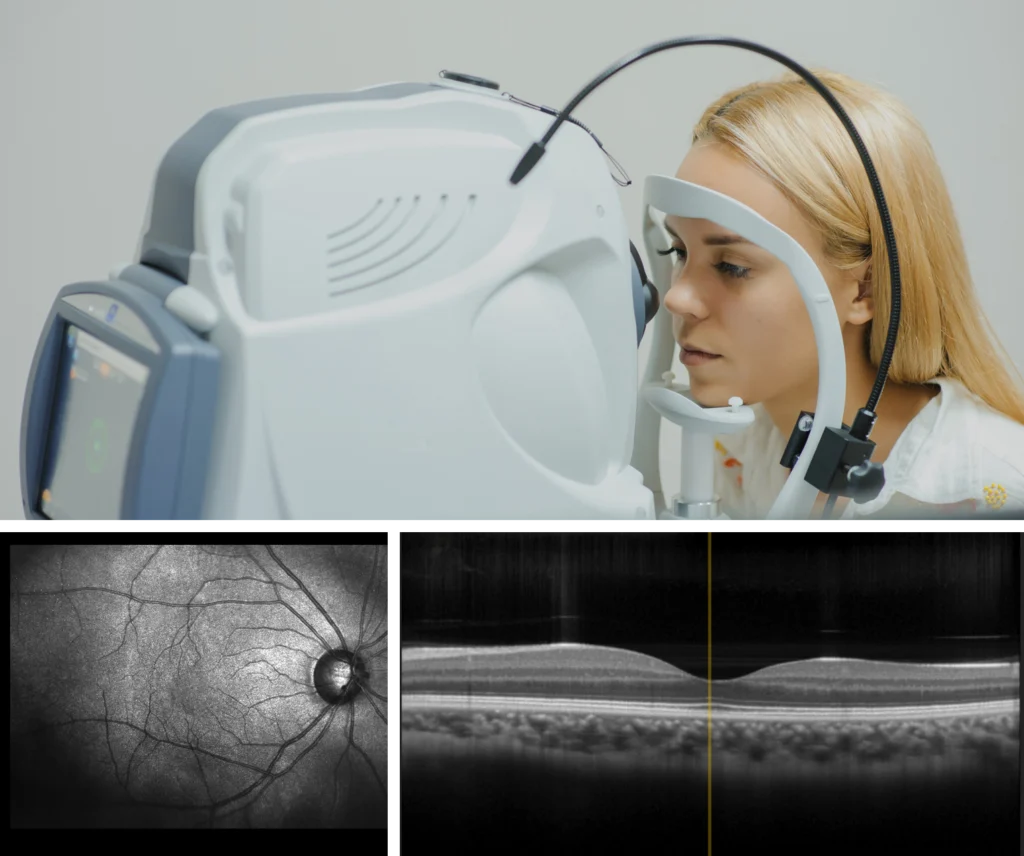
Tests Performed To Evaluate For Diabetic Retinopathy.
In order to evaluate diabetic retinopathy, a doctor may perform tests such as dilated retinal examination and optical coherence tomography (a scan to look for swelling in the retina (DME). In some patients they may perform a fluorescein angiography or a b-scan ultrasound.
In a fluorescein angiography, a dye is injected into the arm, from which to travels through the blood to the eye. Photographs are taken of the eye which map out all the blood vessels and blood flow in the retina. This test identifies areas of blood flow loss as well as areas of new blood vessel grown (neovascularization).
A b-scan ultrasound is a painless procedure whereby an ultrasound is performed over the closed eyelid to evaluate the retinal anatomy in eyes where hemorrhage prevents visualization of retinal details through the eye exam alone
Treatment for Diabetic Retinopathy
The first measure of treatment in diabetic retinopathy is to control blood glucose levels. This will not prevent or reverse diabetic retinopathy, but tends to slow its progress. Doctors can use laser photocoagulation to treat macular edema, placing small burns around the retina’s center, known as the macula. Alternatively, doctors may inject drugs such as ranibizumab (Lucentis), bevacizumab (Avastin), aflibercept (Eylea), or steroids into the eye, in a treatment known as an intravitreal injection. Similar to the pills or Insulin that are necessary to manage one’s diabetes, these injections may be necessary to manage the complications of the disease for years to come.
Doctors and patients can determine the most suitable treatment methods based on the patient’s severity and the macular edema’s precise location. Often, intravitreal injections must be repeated in order to control the macular edema. Proliferative diabetic retinopathy is generally treated with laser photocoagulation, where laser burns are placed in the peripheral retina, but can also be augmented with intravitreal injections. This treatment creates a lower oxygen demand for the retina, either reducing or totally resolving retinal and optic nerve neovascularization. Both forms of treatment can be performed in an office setting.
In treating diabetic retinopathy, early detection is imperative. Treatment is much easier and less invasive in the earlier stages and timely treatment of diabetic retinopathy is the best way to guard against progressive vision loss. Although keeping one’s blood sugars under control does not guarantee good vision, it can reduce the risk of blindness compared to those patients who don’t control their blood sugars.
Treating Vitreous Hemorrhage And Retinal Detachment From Diabetic Retinopathy
In cases of vitreous hemorrhages or traction retinal detachment, a patient may require a surgical procedure known as vitrectomy. Unlike intravitreal injections or laser photocoagulation, vitrectomy is performed in an operating room.
In some case, a vitreous hemorrhage may resolve on its own. Observation is therefore an option, especially in eyes without dense hemorrhage or very severe PDR. Injections of anti-VEGF drugs may be given, and after the hemorrhage resolves, laser may be performed (laser cannot be performed through hemorrhage). If the hemorrhage fails to clear or other complications are noted, surgery may be indicated.
To treat a vitreous hemorrhage, a pars plana vitrectomy surgery may be performed. In this procedure, the hemorrhage is removed, the traction from the new blood vessel (neovascularization) membranes is relieved, and laser is applied to allow the neovascularization to regress. An injection of anti-VEGF medication may be given prior to surgery to reduce intraoperative and postoperative complications risk.
A pars plana vitrectomy surgery may also be performed to treat retinal detachment from diabetic retinopathy. The traction from the new blood vessel (neovascularization) membranes is relieved such that the retina is no longer under traction. Laser is applied so that the neovascularization membranes can regress and new membranes do not form
The eye may be left with a gas bubble or an oil bubble to support the retina during the recovery process. Gas resolves on its own, while oil requires another surgery in the future for removal. An intravitreal injection of anti-VEGF medication may be administered pre-operatively to reduce the risk of intraoperative and postoperative complications/
Stable detachments that do not involve the central vision may be observed for progression. They can remain stable indefinitely
Who Is Most Affected By Diabetic Retinopathy
Individuals with both Type 1 and Type 2 diabetes are vulnerable to the disease. The excessive blood sugar levels can cause the small blood vessels to expand and burst. If you are diagnosed as pre-diabetic, you may also be at higher risk of developing the condition if you develop diabetes later on.
Contact Our Retina Doctors Today
If you have diabetes, it’s important to have your pupils dilated by an eye care professional and if diabetic retinopathy is diagnosed, seeing a retina specialist such as Retina Associates of Orange County can be important in the prevention of further vision loss. Contact the Retina Associates of Orange County to schedule your appointment today.
Common Questions About Diabetic Retinopathy
Diabetic retinopathy is a complex disease, and it can be tough to understand. Many patients have questions about the disease and what to do if they are diagnosed with the disease, such as:
- Is the condition reversible?
- What treatments are available for me?
- What are some of the most common early symptoms?
- Can I reduce my risk of developing diabetic retinopathy?
If you have difficulty understanding any part of diabetic retinopathy, an eye doctor will gladly answer your questions and address your concerns. Having a basic understanding of this disease can help you better understand your diagnosis and what you can do moving forward to reduce the health impact and long-term consequences.
Preventing Diabetic Retinopathy
If you have been diagnosed with diabetic retinopathy, there are some ways that you can prevent the disease. In addition to treatments suggested by your doctor, you can implement many lifestyle changes. Managing your sugar level so that it is healthy is the best way to prevent diabetic retinopathy. Watch your sugar consumption and make sure that you are not consuming too much sugar on a daily basis. Significantly reducing your sugar intake or cutting out certain types of foods with a high amount of sugar from your regular diet can greatly cut your chances of reducing diabetic retinopathy. Consider talking to a nutritionist or other health professional who can help you make necessary dietary changes or adjustments.
When To See an Eye Doctor
As soon as you spot signs of diabetic retinopathy, do not wait too long to set up an appointment. See a doctor right away because it is the only way to understand the severity of your symptoms. A Laguna Hills diabetic retinopathy specialist will do a variety of diagnostic tests so that they can see how far your disease has advanced. The earlier you do so, the higher your chances of successfully treating the disease will be.
You should see a doctor who has specific experience treating patients who have diabetic retinopathy. It is a highly specialized disease, so you will need to see a doctor who is highly familiar with the symptoms and most suitable treatment options that can greatly alleviate your symptoms and improve your vision.
Schedule a Consultation With a Specialist
There are treatment options available if you have diabetic retinopathy. If you meet with a doctor as soon as you can, you can receive the urgent treatment that you need to better manage your condition. Talk to a reputable and competent eye doctor who treats Laguna Hills diabetic retinopathy patients in your area now.
Treatment For Diabetes-Related Eye Conditions
Living with diabetes requires careful management of your health, including paying close attention to your eyes in case of diabetic retinopathy. Diabetes can affect your vision in several ways, but at Retina Associates of Orange County, we’re committed to helping our patients manage their eye health effectively. We’ve received numerous awards for our efforts, including “Top Doctors in Orange County”, and “Best Doctors of America”. Contact us today to get started.
1. Comprehensive Eye Exams
Regular eye examinations are fundamental for anyone with diabetes. These exams allow us to catch changes in the eyes early and start treatment promptly. We recommend that our patients with diabetes have a thorough eye exam at least once a year, or more frequently if recommended.
2. Blood Sugar Control
Managing your blood sugar levels is a critical part of treating eye conditions related to diabetes. High blood sugar can lead to changes in the blood vessels of the eyes and can cause them to leak or become blocked. Keeping your blood sugar within your target range can help protect your eyes from further damage.
3. Blood Pressure And Cholesterol Management
High blood pressure and elevated cholesterol can exacerbate eye problems in diabetic patients. By keeping these under control, you can reduce the risk of vision impairment. We often work in conjunction with your primary care physician or endocrinologist to ensure all aspects of your diabetes are managed.
4. Medications
Certain medications can be used to treat diabetes-related eye conditions. These include anti-VEGF injections, which help to reduce swelling and improve vision by blocking a protein that causes abnormal blood vessels to grow and leak fluid. Steroid injections and laser treatments might also be recommended depending on the specifics of your condition.
5. Laser Therapy
Laser treatment, or photocoagulation, involves the use of laser light to seal or destroy growing or leaking blood vessels in the retina. This procedure can prevent further vision loss and stabilize vision by reducing swelling and leakage. It’s commonly used in various stages of diabetes-related eye conditions to slow progression and preserve eyesight.
6. Vitrectomy Surgery
In advanced cases where there is bleeding in the eye or significant vision loss due to retinal detachment, a surgical procedure called vitrectomy may be necessary. This involves removing the vitreous gel from the eye to prevent it from pulling on the retina and to clear up any blood that may be clouding vision.
7. Regular Monitoring And Follow-Up
Consistent follow-ups are a must for patients dealing with diabetes-related eye conditions such as diabetic retinopathy. Regular monitoring allows us to assess the effectiveness of your treatment plan and make adjustments as necessary. It also provides an opportunity to address any new symptoms that may arise quickly.
Let’s Get In Touch
At Retina Associates of Orange County, we’re dedicated to providing the best possible care to our patients. If you are experiencing any changes in your vision or have been diagnosed with diabetes and have not had a recent eye exam, we encourage you to contact us today. Get in touch with our team, and see how we can help with your diabetic retinopathy.
Posted onTrustindex verifies that the original source of the review is Google. Cannot say enough about the level of expertise and competency of Dr Hwang and his staff. He saved my vision by repairing a detached retina in my right eye and has been providing incredible care in treating my macular condition and retaining my vision over the years. He is caring and compassionate with a true love for his practice. I am blessed to be one of his patients!Posted onTrustindex verifies that the original source of the review is Google. Check up on visual issue went perfectly. Great staff as well.Posted onTrustindex verifies that the original source of the review is Google. Professional and thoughtful doctor, caring patient as a family member.Posted onTrustindex verifies that the original source of the review is Google. Great service. Very satisfied.Posted onTrustindex verifies that the original source of the review is Google. I have tremendous anxiety prior to my intraocular injections to manage my wet AMD, but Dr. Hwang makes the process as quick and painless as possible. I wouldn't trust my eye health to anyone else. He's the best.Posted onTrustindex verifies that the original source of the review is Google. The receptionists are very courteous. Appointments are always on time. Dr. Hwang answers all questions and explains things to you.Posted onTrustindex verifies that the original source of the review is Google. Always good service. Dr. Gupta is first rate.