Newport Beach Macular Pucker
Macular Pucker or Epiretinal Membrane
 Macular pucker affects approximately 10 percent of people, particularly men and women over the age of 50. Based in the center of your retina, the macula is responsible for the part of your vision that allows you to see straight ahead. As you read the text on this page, you are using your macula. When the retinal surface forms an extra layer of tissue and contracts, distorting the retina, it is known as a macular pucker. They look like a piece of scotch tape and can distort the central vision. If you start to notice this, you should see a doctor for macular pucker as soon as possible.
Macular pucker affects approximately 10 percent of people, particularly men and women over the age of 50. Based in the center of your retina, the macula is responsible for the part of your vision that allows you to see straight ahead. As you read the text on this page, you are using your macula. When the retinal surface forms an extra layer of tissue and contracts, distorting the retina, it is known as a macular pucker. They look like a piece of scotch tape and can distort the central vision. If you start to notice this, you should see a doctor for macular pucker as soon as possible.
The Retina Associates of Orange County
If you live in Newport Beach macular pucker doctors are nearby. The Retina Associates of Orange County are licensed and certified ophthalmologists in California. Our multilingual staff (Tagalog, Korean, Chinese, Vietnamese, English, Farsi, and Spanish) helps clients of all ages and from different backgrounds. We see a broad range of eye problems including macular pucker. Guided by our knowledge, experience, and passion to enable people to improve their vision, we have a built a solid reputation. If you are in Newport Beach macular pucker consultations are just a phone call away.
Understanding the Macula
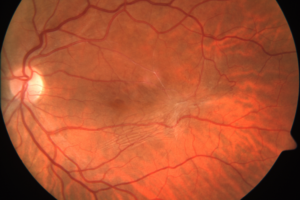
The retina is the light-sensing layer of cells that lines the inner wall of the back of the eye. The macula is the center of the retina that allows one to see fine detail. If you think of your eye like a camera, the retina and macula are the film of the camera. There are many conditions that can damage the macula.
An epiretinal membrane is a condition with many names: macular pucker, pre-retinal fibrosis, cellophane maculopathy, and surface wrinkle retinopathy, among others. All of these allude to an ailment that causes blurred and/or distorted central vision.
What causes an epiretinal membrane or macular pucker?
The vitreous gel separates from the retina in nearly everyone at some point in his or her life. In some people, when the vitreous separates, it causes scar tissue to form over the macula. This extra tissue will often thicken and contract, causing an irregular surface of the macula layer.
What are the symptoms of an epiretinal membrane or macular pucker?
Some patients are without symptoms, but as the macular pucker or epiretinal membrane thickens, patients will often describe wavy lines or distorted central vision. Blurred vision and/or difficulty reading may also be a symptom.
Macular Puckers versus Macular Holes
A macular pucker and macular hole are different conditions of the eye. Both result from a shrinking vitreous pulling on the retina. When this pulling leads to small microscopic damage, the retina can naturally heal itself, but the scar tissue that results can be considered a macular pucker. If the shrinking vitreous pulls on the retina too hard, a tear can result. Known as a macular hole, this is a more serious condition. Both issues present similar symptoms which is why you should see an ophthalmologist for an accurate diagnosis and proper treatment.
Diagnosis
An ophthalmologist can examine your retina in order to diagnose an epiretinal membrane. Once the membrane is detected, there are two common photographic tests administered for assessing the extent of the damage to the underlying retina. These tests are fluorescein angiography (FA) and optical coherence tomography (OCT).
Fluorescein Angiography– in a in a fluorescein angiogram, patients are injected with sodium fluorescein dye through the veins in their hands or arms. Then the physician takes a series of photographs of the retina. The physician can use these photographs to evaluate the retinal layer, the layer beneath the retina and the retina’s blood vessels. The dye used in this process is not x-ray dye and no x-ray is taken. Rather, sodium fluorescein dye is a photographic dye that the patient will eventually eliminate from the body through urination. The dye may stain the patient’s skin yellow for up to 24 hours. The test is considered highly safe and effective. However, some patients may prove allergic to the dye. In this case, another kind of test, optical coherence tomography, may be administered.
Optical coherence tomography is a newer epiretinal membrane assessment in which light waves are bounced off the retina to obtain a cross section image. No dye is used in this exam. Rather, the light waves map the retina, acting similarly to sonar waves mapping images of the ocean floor.
Epiretinal Membrane Treatment
The only way known to treat epiretinal membranes is to surgically remove them. Surgery is generally not necessary in cases where symptoms are mild. If both eyes are affected, strengthening one’s bifocals or using a magnifying glass may improve one’s near vision.
In more substantial cases, the membrane is removed in a procedure known as vitrectomy. This is generally an outpatient procedure in which local anesthesia is administered. Surgeons in this procedure use minute instruments to remove the vitreous humor from the eye’s central cavity and then remove the membrane that wrinkles the macula. After which, the macula should smooth out and symptoms will gradually be reduced. Most patients see an improvement in vision following this treatment. However, vision usually does not return to normal, and some visual distortion and reduced acuity often remain.
As with any surgery, there are risks. In vitrectomy surgery, the risks include infection, bleeding, torn or detached retina, inflammation, or affects to the blood vessels in the retina.
How successful is Newport Beach macular pucker surgery?
Repairing a macular pucker with a surgical procedure is a delicate process. In most cases the vision will improve; however, sometimes it does not return to normal. Every patient is different; some will see a large improvement and others only slightly. That being said, the majority of patients will see an improvement in vision distortion. Recovery can take three months or more. It’s important to follow any recommended post surgical treatment for optimal outcomes.
Other Conditions of the Eye in Conjunction with Macular Pucker
When you visit Newport Beach macular pucker doctors, you may also be examined for additional diseases of the eye. Oftentimes, patients with macular pucker will have other eye problems including cataracts, macular edema, or retinal vein occlusion. If any of these issues are discovered, a treatment plan will be devised that includes each problem. Some can be addressed and treated simultaneously and others will need to be individually treated when the time is right. Your ophthalmologist can discuss all of your options during your eye appointments. Rest assured that when you are a patient of the Retina Associates of Orange County, you will be in good hands.
Contact Us Today For Treatment of Macular Pucker or Epiretinal Membrane
If you suspect you are suffering from visual distortion caused by epiretinal membranes, contact Retina Associates of Orange County. Our qualified retinal specialists can help restore your sight and/or prevent further vision loss.
Whether you are in Santa Ana, Laguna Hills, or Newport Beach macular pucker doctors can help you correct and restore your vision; call us at 949-706-3514 for a free consultation.
Common Symptoms of Macular Pucker
As a certified eye doctor who provides Newport Beach macular pucker treatment services can explain, there are several symptoms to look out for. Certain people are more prone to developing macular pucker later in their life. People can develop a macular pucker, or build up of tissue, due to a number of reasons, such as diabetes or even a serious personal injury accident. While some people experience no symptoms at all, others have one or more serious symptoms that can greatly impede their vision. Being aware of the common symptoms of macular pucker can help you seek treatment sooner once you notice them. If you experience two or more of the following symptoms and they have persisted for several days, you may want to see an eye doctor right away.
Blurry Vision
The macula is the part of the area that allows you to perceive objects with sharp detail. Because of the build-up of tissue that develops on the macula, the macula becomes obstructed. This can cause your vision to become blurry. The severity of blurry vision as a result of macular pucker can range from slight vision loss to severe vision loss, depending on each individual. However, for some people with mild blurry vision, they may not need to go through extensive treatment. If you feel like you are having difficulty viewing objects or you are struggling to read small text or make out finer details, it could be an indicator that you have a macular pucker.
Wavy Lines
Another common symptom of a macular pucker are wavy lines. Many people who have macular pucker notice that straight lines are wavy because they are distorted. For example, if they view a barcode, they may see that the black lines are way rather than straight. Because the macula has an excess of tissue, it affects the brain’s ability to process images and visual cues. Individuals with macular pucker have their central vision affected, making it hard to put things in focus. This distortion may also be even more noticeable at night, such as when a person is driving their car and they view the reflection of lights.
Gray Spots
People with macular pucker also commonly report the sudden onset of gray spots or blind spots. This symptom can greatly affect vision, and can make it unsafe to do essential activities such as driving, using tools, or operating machinery. If you feel like you are seeing gray spots that are obstructing your vision, it could be a sign of a macular pucker. A gray spot develops when there is a gray or cloudy portion on the middle of the eye surface. It can look like multiple small shadowy blobs that come and go. If the gray spots continue to bother your vision, you may want to speak to an experienced Newport Beach macular pucker specialist.
A macular pucker can develop in one or both eyes, so if you notice anything wrong with your vision at all and the issues have persisted for several days, you may want to see an eye doctor for an exam right away. To learn more about Newport Beach macular pucker services available near you, schedule a consultation with a trusted eye doctor right away.
Risk Factors For Cellophane Maculopathy
Understanding the risk factors associated with Cellophane Maculopathy (often known as macular pucker) is vital if you want to maintain healthy vision. At Retina Associates of Orange County, our award-winning ophthalmologists leverage their extensive training and experience to provide personalized patient care with cutting-edge treatment options. Now, we’re ready to help you. Read on to learn more about common risk factors of cellophane maculopathy, and contact us today to get started on your treatment.
1. Age
Age is a significant factor, with most cases of Cellophane Maculopathy occurring in individuals over the age of 50. As we age, natural changes in the eye can lead to the formation of a thin film over the macula, affecting vision quality.
2. Diabetic Retinopathy
Individuals with diabetic retinopathy are at a higher risk of developing Cellophane Maculopathy. High blood sugar levels can damage blood vessels in the retina, potentially leading to the formation of scar tissue and subsequent visual impairment.
3. Eye Surgery
Previous eye surgeries, particularly those involving the vitreous or retina, can increase the risk of developing Cellophane Maculopathy. Surgical procedures can lead to changes in the eye’s internal structures, sometimes resulting in scar tissue development.
4. Trauma To The Eye
Any form of trauma to the eye, such as a blunt force injury, can precipitate the formation of scar tissue on the macula. This scar tissue can contract and cause the retina to wrinkle or pucker, impacting vision.
5. High Myopia
Highly nearsighted individuals are more likely to develop conditions related to the vitreous and retina, including Cellophane Maculopathy. Nearsightedness can cause stretching and thinning of the retina, making it more susceptible to abnormalities.
6. Vascular Conditions
Certain vascular conditions that affect blood flow, such as hypertension and vascular blockages, can also increase the risk of this condition. Poor circulation can lead to the accumulation of fluid and the formation of membranes that can disrupt the normal retinal structure.
7. Inflammatory Eye Conditions
Inflammation within the eye, such as from uveitis or posterior vitreous detachment, can contribute to the formation of epiretinal membranes. Chronic inflammation can lead to the proliferation of cells that form scar tissue on the retina.
8. Lifestyle Factors
Lifestyle factors such as smoking can contribute to overall vascular health and may indirectly increase the risk of developing macular pucker. Maintaining a healthy lifestyle with regular exercise and a balanced diet can help reduce this risk.
Recognizing these risk factors can help in early detection and management of Cellophane Maculopathy. Regular eye exams are crucial for those at higher risk due to age, underlying health conditions, or past eye traumas. If you experience any changes in your vision or fit into the high-risk categories, it’s important to seek professional advice.
Contact Us Today
At Retina Associates of Orange County, we are here to help you with any concerns about your retinal health. Don’t hesitate to contact us for an evaluation if you believe you are at risk or are experiencing symptoms that affect your vision. Let us help you maintain your vision health with our comprehensive care and advanced treatment options. Get in touch with us today, and see how our team can help with macular pucker.
